Perspectives
Finding a Real Solution to the Point Solutions Problem
Today’s employers have plenty on their plate, but rising healthcare costs still top their list. Plus, health inflation-induced costs are estimated to increase by 9-10% through 2026.1
To combat these circumstances, healthcare point solutions continue to hit the market, striving to be the silver bullet for health ailments, health management, member engagement and cost reduction. Venture capital firms continue to fuel this explosion of point solutions for good reason: Half of the nation’s employers have contracts with four to nine point solutions, and many other employers are considering adopting them.3
82% of employers say rising healthcare costs impact their competitiveness2
Meanwhile, some major healthcare plans are buying up their favorite solutions. This can stifle innovation and add to the inflexible nature of healthcare because these players now have vested interest in selling their products—even if they’re not the best or right ones for a population’s needs.
A dizzying array of duties.
On the other side of a crowded market are human resource leaders. They have the difficult task of sifting through the sea of point solutions, working with each vendor and trying to determine if the investment will bring health, as well as cost returns to their employee population—and the company. From the research it takes to properly vet options to the implementation, ongoing management and performance analysis, it becomes a full-time job. One study found that the direct cost of employers sorting through the complexities of health and benefits administration was approximately $21.57 billion.4
Along with the obvious burden, taking on health benefits management can lead to employers sticking with the same point solutions, even if they’re not meeting their employees’ needs.
“Point solutions complicate the entire benefits program. Let’s say I implement a diabetes program. Then I turn around and get a hypertension program and then I decide we are going to add a weight loss program with obesity drugs… and I start doing all these individual things.
It makes my job more challenging. There are more contracts, more communications during open enrollment, and more costs, so determining an ROI becomes more challenging.”
The “promise” of integration.
Integration has been a buzzword for some time now, not only within the health industry, but across most industries.
While everyone likes to tout their ability to integrate, the realities of integration are complex and involve alignment from all parties.
For example, let’s say that a member gets diagnosed with back pain. Their health plan then connects them to a musculoskeletal point solution offered through their work. Unless there is data integration between the health plan and the point solution, the point solution will not have the full picture from the health plan about the member. And as the member engages with the point solution, the health plan will not receive the appropriate updates about the member’s progress. This results in inefficient collaboration between the point solution, the health plan and the member’s care team, a less-than optimal member experience with the potential for less-than-optimal outcomes.
A path to better.
While there is no silver bullet when it comes to healthcare point solutions, there are strategies that support optimal point solution performance and lead to a better experience for employers and members.
Backed by research, Celeste Health Solutions has developed a system and set of best practices to help employers get the most out of their point solutions:
- Break through the clutter
- Streamline the process
- Optimize member engagement
Let’s dive into each.
1. Break through the clutter
While it’s great to have choices, many employers need—and desire—help understanding and narrowing down the dizzying array of options. A carefully chosen selection of high-quality point solutions is like a wardrobe that’s been hand-curated by a personal shopper: everything you need, nothing you don’t and none of your precious time lost in the search. That’s why our Market Solutions team has vetted more than 300 solutions across multiple clinical categories to provide a curated, comprehensive Innovations Hub to meet every employer’s needs.

Clinical categories we regularly review:
- Behavioral Health/SUD
- Diabetes/Metabolic Health
- Engagement/Wellbeing
- Expert Medical Opinion
- Female/Family
- Gut Health/Digestive
- Musculoskeletal
- Oncology
- Pharmacy
- Advanced Symptom Checker
- Cardiology
- CKD/ESRD
- Cost/Quality
- Transparency
- DEI/Health Equity
- Digital Member Communications
- Financial Wellbeing
- High Tech Imaging and Testing
- Incentive-Based Shopping
- In-Home Care
- Medical Devices
- Nicotine Cessation
- Nutrition
- Onsite/Near-Site
- Preventive Check-Ups
- Specialty Med/Rx
- Virtual PCP
Guiding principles
While meticulous research, comparative analysis and discussions with each vendor are key to finding good solution contenders, evaluating each contender against a set of specific criteria provides a more systematic way of review. We use the following six criteria to help determine if a vendor is a good fit:
- Outcomes: Exemplary and measurable, with accountability
- Flexibility: The ability for clients to choose the solutions that fit their distinct needs
- Member Experience: Simplicity, encouragement, advocacy, personalization and authenticity
- Member Empowerment: Providing the proper information and support for members to make the best decisions
- Membership: Designed to help members feel like they are a part of something special and meaningful
- Experimental: Innovating quickly and demonstrating agility
Neutrality
Once a solution is added to the mix of options, its performance should be regularly measured to ensure it continues to work well for a population’s needs. If it stops meeting expectations, having the ability to quickly replace it is important. While some industry players have vested interest in specific solutions, our Innovations Hub serves as a neutral third party so that the point solutions being offered are always in the best interest of employers and their members. This neutrality spurs healthy competition and accountability, as well as underscores the importance of performing ongoing market research to identify new, innovative solutions as they become available.
Tailored Attention
A curated selection of point solutions is an immense help in narrowing down options, but employers still need to choose the solutions that are right for their population. To support them in this effort, Celeste scours each employer’s data to deeply understand which point solutions align with their needs, along with which fit best together, and then pairs that with in-depth consultation. Factors such as the cost, ROI, longitudinal progression of disease, existing comorbidities, relationship to healthcare, engageability and social determinants of health are considered, among others.
2. Streamline the process
Simplified integration
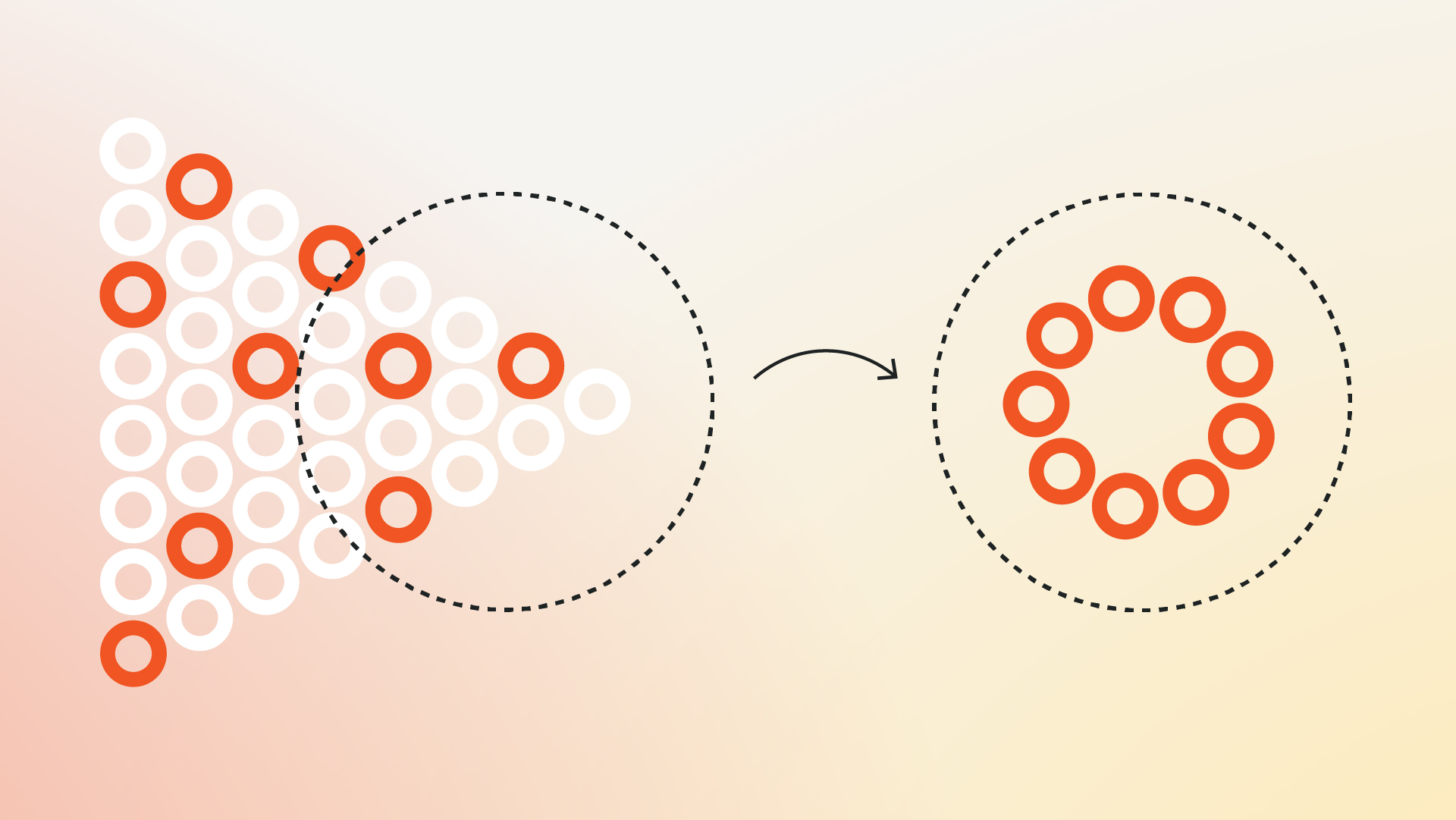
The more point solutions an employer decides to offer, the more work for them on the backend. To solve this, Celeste contracts directly with each point solution and establishes powerful data integration, enabling Celeste to streamline and manage the entire administrative process. This in turn means employers go from dealing with multiple vendors to partnering with just one (Celeste).
Taking this huge responsibility off the employer saves two very important things: time and money. It also strengthens point solution effectiveness and engagement.
Consolidated contracting, billing and eligibility
- One contract and streamlined billing
- Favorable market pricing driven by large-scale purchasing power and pre-negotiated rates
- Coordination of all member eligibility requirements across solutions
Turnkey plug-and-play implementation
- Quick uptake and streamlined go-live
- Flexibility to change and add solutions
- Flexibility to integrate with an employer’s current vendors
Targeted and customized clinical outreach strategies
- Deep analysis within population segments
- Development and implementation of targeted strategies
Consolidated communications
- Boosts member clarity and engagement
- Tailored messaging based on different employer needs
- Provides support to HR employees
Aggregated reporting and independent ROI assessment
- Corrects for bias
- Simplifies performance measurement
- Ensures accountability across key vendor partners
3. Optimize member engagement
As mentioned earlier, the member experience is an important consideration when vetting and securing the right point solutions. However, like most things, point solutions are not used in a vacuum. Typically, they are one of many benefits that an employee has access to. And so when it comes to members actually engaging with them in the context of real life, it becomes tricky.
Let’s say, for instance, that an employee at a trucking company is diagnosed with diabetes. Very quickly, their list of healthcare touchpoints and to-dos can become overwhelming:
- PCP
- Endocrinologist
- Pharmacist
- Diabetes point solution
- Medical insurance
- Retail pharmacy insurance
If they deal with comorbidity, that list continues to grow, and it is easy to see how someone with health issues could have a hard time managing their health.
Having an orchestrator at the center can greatly improve efficiencies and the experience. Celeste’s Care Advocates exist for this very reason. Like an air traffic controller, Care Advocates are plugged into a member’s healthcare data, touchpoints and full array of benefits to help them seamlessly coordinate and manage their health. In the case of the employee diagnosed with diabetes, the Care Advocate serves as the member’s central point of contact, helping them establish doctor’s appointments, connecting them to the right specialists and point solutions, and answering questions about medical bills, insurance claims or benefits.
Two-way communication between members and Care Advocates takes place over the phone, as well as within the member app where each member has access to a personalized care plan that outlines their next-best actions.
The main takeaway? Celeste helps members use the correct benefit at the correct time—point solution or otherwise—in the context of all other benefits.
Beyond the Innovations Hub, Celeste integrates with virtual primary and mental health care. This means that both the Care Advocates and the virtual PCPs are keyed in on any point solutions a member is eligible for or using, and can help members use point solutions to their full potential. Ultimately, this leads to better member engagement and a better member experience.
Conclusion
During the time you’ve taken to read this report, it’s possible that another point solution has been ideated or hit the market.
While point solutions continue to provide innovative remedies to healthcare challenges, cashing in on their full potential is difficult for employers and members alike.
For employers, having a partner who can remove decision fatigue, provide an integrated hub of highly curated options, deliver tailored consultation, ensure optimal engagement and make the administrative process easy is extremely powerful. Not only does it free up an employer’s time, it leads to better point solution ROI.
For members, having convenient health solutions that cover their spectrum of needs and a guide to help them navigate and utilize their benefits to the fullest has a substantial impact on their experience and their outcomes.
Sources:
- https://www.mckinsey.com/industries/healthcare/our-insights/the-gathering-storm-the-threat-to-employee-healthcare-benefits
- https://www.managedhealthcareexecutive.com/view/employer-survey-finds-high-cost-claims-and-hospital-prices-are-major-concern
- https://healthpayerintelligence.com/news/2024-employer-sponsored-health-plan-predictions-glp-1s-vendors-data
- https://journals.aom.org/doi/full/10.5465/amd.2020.0063

